-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Ahmed H Al-Darraji*
Corresponding Author: Ahmed H Al-Darraji, Assistant Professor of Pharmacology College of Pharmacy University of Basrah, Iraq.
Received: July 09, 2024 ; Revised: July 12, 2024 ; Accepted: July 15, 2024 ; Available Online: August 14, 2024
Citation: Al-Darraji AH. (2024) Evaluation the Hesitancy of COVID-19 Vaccination Process in a Large-Scale Survey in Iraq. J Pharm Sci Drug Discov, 3(1): 1-12.
Copyrights: ©2024 Al-Darraji AH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Background: Vaccination is crucial to reduce the pandemic spread of SARS-CoV- 2/ coronavirus disease 2019 (COVID-19). Therefore, besides the development and supply of vaccines, it is essential that sufficient individuals are willing to be vaccinated. However, a large proportion of populations all over the world shows vaccination hesitancy. This makes it is important to determine factors that prevent vaccine acceptance.
Materials and Methods: This is a cross-sectional study that was conducted from 8 January 2022 to 30 Jun 2022. The sample of population was a convenience sample targeted through a digital campaign using social media platforms (more than 780 responders). Our survey consists of 29 questions, capturing demographic data, acceptance of COVID-19 vaccine, attitudes toward the need for COVID-19 vaccination and associated health policies, and reasons for vaccination hesitancy.
Results: We found that 56.3% (440) of our sample population believe that vaccines are safe and effective against COVID 19 and reduce infection risk. A very high percentage (about 80.1%) of people (626) believe that all population, regardless of age and health condition, should take the vaccine to minimize infection symptoms. Around 80.9% (633) believes that taking the vaccine is a part of taking care of themselves.
Discussion: Vaccines have become the best weapon for epidemic prevention and control in the absence of standard approved effective therapies. However, skepticism about the vaccine efficacy and safety is constantly reported. To our knowledge, there is not enough number of studies that assess COVID- 19 vaccine process. The primary objective of this survey is to assess COVID-19 vaccination process in Iraqi people.
Keywords: COVID-19, Vaccines, Survey, Infection risk
INTRODUCTION
Coronaviruses, which infect both animals and humans, are a group of viruses that belong to Coronaviridae family. In humans, the severity of the infectious disease caused by these viruses may result in a mild form, such as common cold, to a very sever illnesses, such as MERS (Middle East Respiratory Syndrome) and SARS (Severe Acute Respiratory Syndrome) [1,2].
A new generation of coronavirus that has never been recognized in humans before emerged in Wuhan, China in December 2019. The new one is now called the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 2019-nCov HCoV-19), and the disease caused by this virus is known coronavirus disease 2019 (COVID-19). This new virus became a global pandemic as of January 2020 and is continuously active as of February 2022. Almost 428 million COVID-19 cases have been diagnosed around the world with ~ 5.91 million deaths as of February 2022 [3].
It is essential to notice that COVID-19 is a virus and using drugs such as antibiotics, supplements, or antiparasitic drug (ivermectin) is not very helpful to treat this infectious disease. Obviously, treating of virus and bacterial infection are completely different. Using antibiotics to treat viral infection could reduce the risk of secondary bacterial infection; however, it could cause unwanted effects or, unfortunately, increase the prevalence of antibiotics resistance [3].
Medications that have been commonly used for COVID-19 in Iraq could include antimicrobials (azithromycin, levofloxacin, ceftriaxone, chloroquine), antipyretics and analgesics (paracetamol), anticoagulants, bronchodilators, corticosteroids, fibrinolytics, immunomodulating agents, and some miscellaneous drugs (colchicine, ivermectin). Though supplements and vitamins have been also used to enhance the immune system function, they do not prevent or cure COVID-19 infections. There is no effective treatment for COVID-19 infections and the previously used drugs are merely employed to minimize symptoms and improve immunity. The most effective methods to control COVID-19 maintain personal hygiene and full vaccination [3,4].
Three main approaches are considered to designing a new vaccine for COVVID-19. They are different in whether they use the whole entity of virus, or just parts of the virus body (antigens) that induce the immune system or using only genetic materials (blueprint) that are necessary for making certain proteins and not the whole virus. Regardless of whether approach is used to synthesize COVVID-19 vaccine, this weakened version of virus would never cause COVID-19 infection in individuals receiving the vaccine. It will enhance the functions of immune system in vaccinated people to respond much faster and stronger when they expose to the actual pathogen for the first time. The most used COVID-19 vaccines include: AstraZeneca** (Vaxzevria), Moderna. Spikevax, Janssen (Johnson & Johnson) Ad26.COV2S, Covovax™, Covishield™, Covaxin®, Nuvaxovid™ (Novavax), Sinovac** (CoronaVac) Sinopharm/BIBP [5-7].
The COVID-19 pandemic had a significant impact on Iraq starting in early 2020. The Iraqi government implemented a range of measures to try to control the spread of the virus, including lockdowns, curfews, and the closure of schools and businesses. However, the pandemic exacerbated the existing challenges Iraq was facing, including a fragile healthcare system, economic instability, and political divisions. Iraq began its COVID-19 vaccination rollout in March 2021, initially focusing on priority groups like healthcare workers and the elderly. The rollout was hampered by limited vaccine supply, logistical challenges, and vaccine hesitancy among the public. By the end of 2021, only around 15% of the Iraqi population had received at least one dose of a COVID-19 vaccine [8].
In 2022, the Iraqi government sought to ramp up its vaccination efforts, implementing public awareness campaigns and working to expand vaccine availability nationwide. However, vaccination rates remained relatively low, with just around 25% of the population fully vaccinated by mid-2023. Throughout the pandemic, the Iraqi government issued a range of policies and guidelines to try to control the spread of COVID-19, including lockdowns, curfews, mask mandates, and restrictions on gatherings and travel. Enforcement of these measures was uneven, and the policies often faced pushback from segments of the Iraqi public. Public health authorities in Iraq also launched various awareness campaigns to encourage mask-wearing, social distancing, and vaccination. However, these efforts were challenged by misinformation, conspiracy theories, and skepticism among some Iraqis about the threat of COVID-19 and the safety and efficacy of vaccines [8].
Three vaccines are available in Iraq. The first one is Pfizer/BioNTech (Comirnaty®) which requires two doses. It is an mRNA vaccine that activates immune response against COVID-19 through making new proteins. The second one is AstraZeneca (Vaxzevria)R that requires two doses as well. This one is a type of viral victor vaccine. The last one is Sinovac (CoronaVac)R and Sinopharm/BIBP that also requires two doses. This vaccine is a type of inactivated vaccine with an adjuvant. In this regard it is unique to the virus that causes COVID-19; however, it is much less effective than other vaccines [8].
Since the advent of vaccines and their commercial availability, there has been a persistent undercurrent of skepticism and resistance. These sentiments have only intensified with the advent of the Internet and social media, which have facilitated the rapid dissemination of vaccine-related controversies. This surge in vaccine hesitancy has coincided with concerning outbreaks of vaccine-preventable diseases in populations that remain unvaccinated or under-vaccinated. The public health implications of these trends are dire and demands immediate attention. Over the past decade, substantial research has been dedicated to understanding the causes, consequences, and impacts of vaccination hesitancy. However, despite these efforts, there is still an urgent need for more in-depth research to fully comprehend and address public apprehensions surrounding vaccines. The past two years of the COVID-19 pandemic have underscored this need, as uncertainties and debates regarding COVID-19 vaccines have further amplified vaccine hesitancy [9].
To effectively address vaccine hesitancy, it is critical that we conduct focused and comprehensive research aimed at understanding the complex interplay between individual, community, socio-cultural, and political dynamics [9]. We must delve into how indigenous knowledge, beliefs, and socio-cultural influences shape perceptions of vaccines. Moreover, it is crucial to examine how criticisms-whether valid, false, or perceived as true—affect vaccination acceptability and how these concerns can be addressed in a non-judgmental and measured manner. Such research will not only provide a clearer understanding of the underlying issues but also inform the development of targeted interventions and communication strategies. These strategies must be culturally sensitive and designed to build trust and confidence in vaccines and vaccination programs.
To the best of our knowledge, no studies were performed in Iraq to comparing among different vaccines regarding effectiveness, safety, and people perception. Therefor our study aims to fill the gaps by investigating vaccine acceptance using a large-scale survey targeting Iraq population following vaccine availability and administration. Secondly, to unveil the barriers that lead to vaccine hesitancy and its prevalence in the population, we used an extensive updated survey that reveals vaccine acceptance. This work is also to increase the awareness of undereducated groups by directing them to reliable sources of information.
Theoretical Foundations
Our framework draws on several theoretical perspectives to examine vaccine hesitancy:
MATERIAL AND METHODS
We used an open online survey that was conducted using the online platform (https://www.googleforms.com/). This survey was carried out among population in Basra, Iraq. It was conducted from January to June 2022. The sample population was a convenience sample targeted through a digital campaign using social media platforms. Data sampling of 400 respondents was expected, however more than 780 responses were obtained.
Methodology
The survey consisted of 29 questions, capturing demographic data, acceptance of COVID-19 vaccine, attitudes toward the need for COVID-19 vaccination and associated health policies, and reasons for vaccination hesitancy. All questions were written and validated in the Arabic language, English translation below:
STATISTICAL ANALYSIS
The data are analyzed using a combination of descriptive statistics, bivariate analyses, and multivariate regression models to: Identify the prevalence and predictors of COVID-19 vaccine hesitancy, Examine the relative importance of the different theoretical constructs in explaining vaccine hesitancy, Explore the interaction between individual, interpersonal, community, and societal/structural factors. Data are presented as mean. Statistical analyses were performed using the Prism 7 software package (GraphPad, La Jolla, CA).
RESULTS
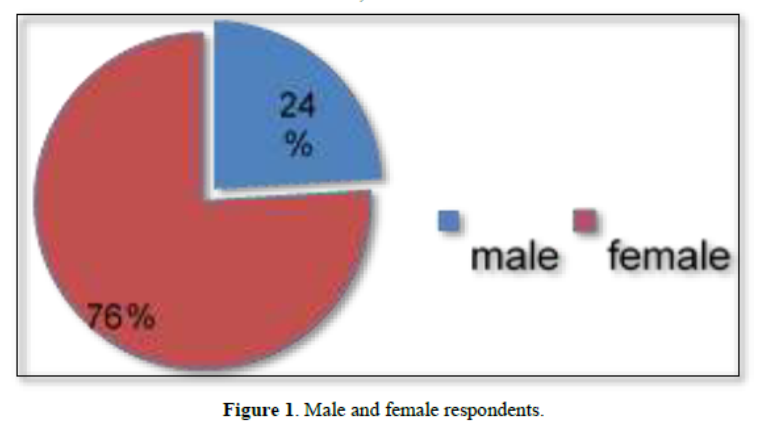
782 respondents, males and female, aged between 19 and 50 years from Iraq residents were in the study. 76 % of the participants were female, while 24 % were males as shown in the Figure 1.
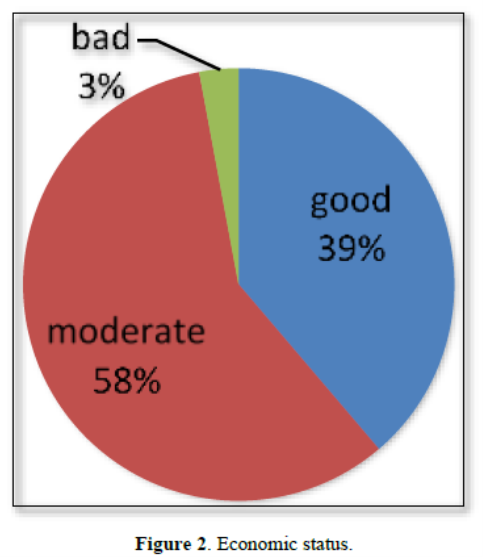
Then we examined the economic status of the participants and found that most of the participants were from a moderate economic level with a percentage of 58.30%. 38.7% were from a good economic status, while the least were from a bad economic state with a percentage of 2.94%, as shown in Figure 2.
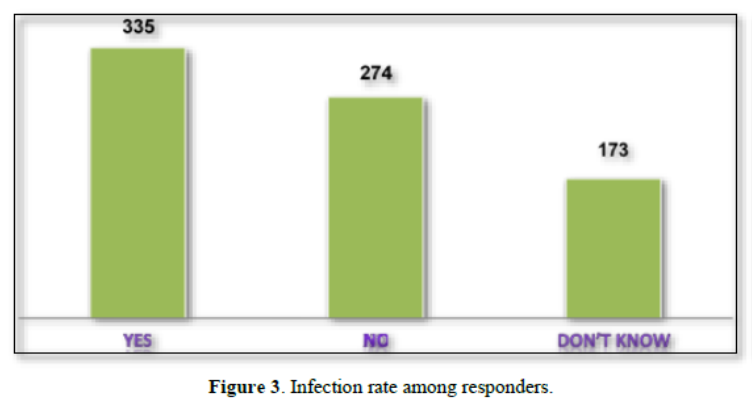
 We also found that 42.84% (335) of the respondents were answered with (YES) when they responded to the question if they had been infected with the virus. While 35.04% (274) answered with (NO) and 22.12%v (173) answered with (do not know), as shown in Figure 3.
We also found that 42.84% (335) of the respondents were answered with (YES) when they responded to the question if they had been infected with the virus. While 35.04% (274) answered with (NO) and 22.12%v (173) answered with (do not know), as shown in Figure 3.
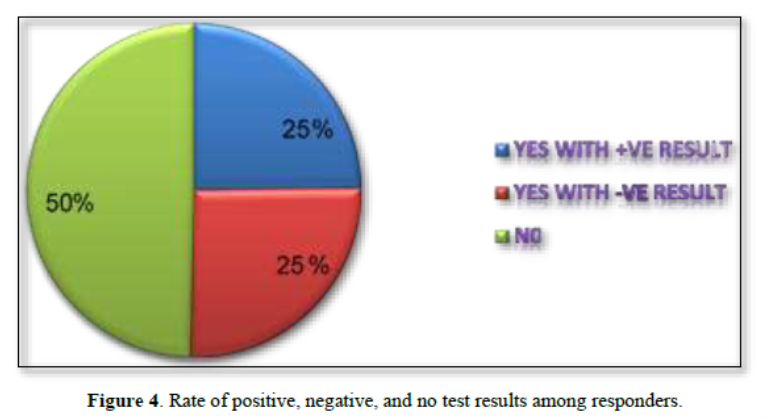
The 782 respondents were also asked if they had been tested for COVID-19, 194 one of them had the test (POSITIVE), 200 were negative, and 388 have not been tested before, as seen in Figure 4.
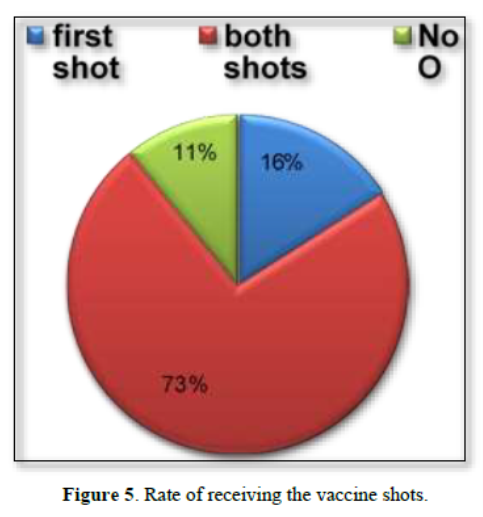
We also found that the percentage of participants who received only the first shot was 16%, both shots 73%, or they did not receive any shots at all 11%, as shown in Figure 5.
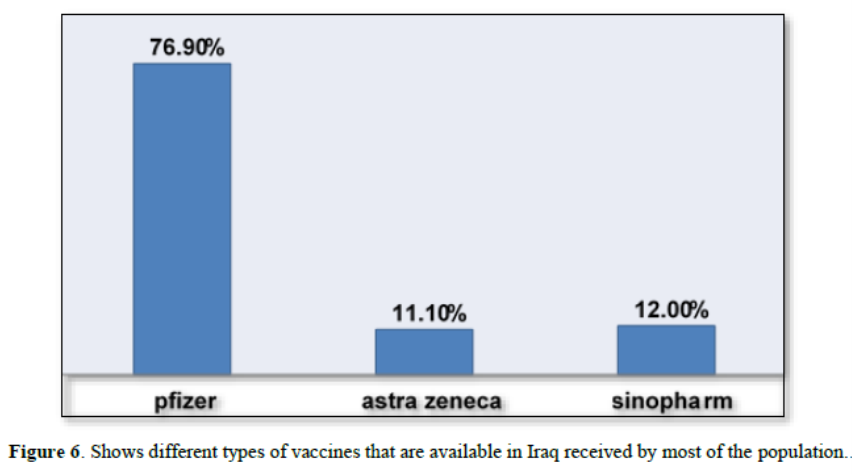
Different types of vaccines that are available in Iraq were received by the population. Pfizer/BioNTech vaccine was the most commonly used one (76.9%) among vaccinated people especially after FDA approval (Figure 6). While AstraZeneca and Sinopharm vaccines with rates of 11.1% and 12%, respectively, among responders (Figure 6).
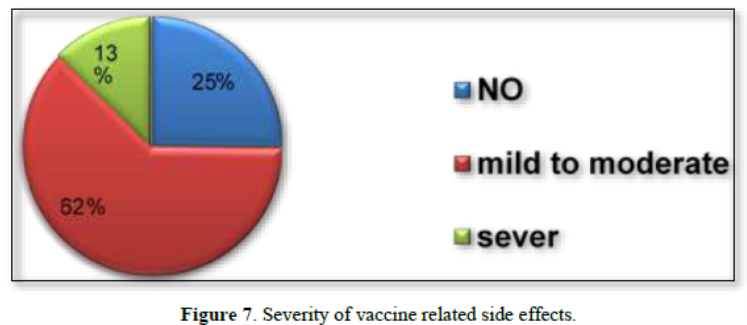
Participants were also asked if they have experienced adverse effects after receiving vaccination shots. A wide range of unwanted side effects, such as fatigue, fever, muscle ache, pain in the injection site, have been reported to us by the participants (Figure7).
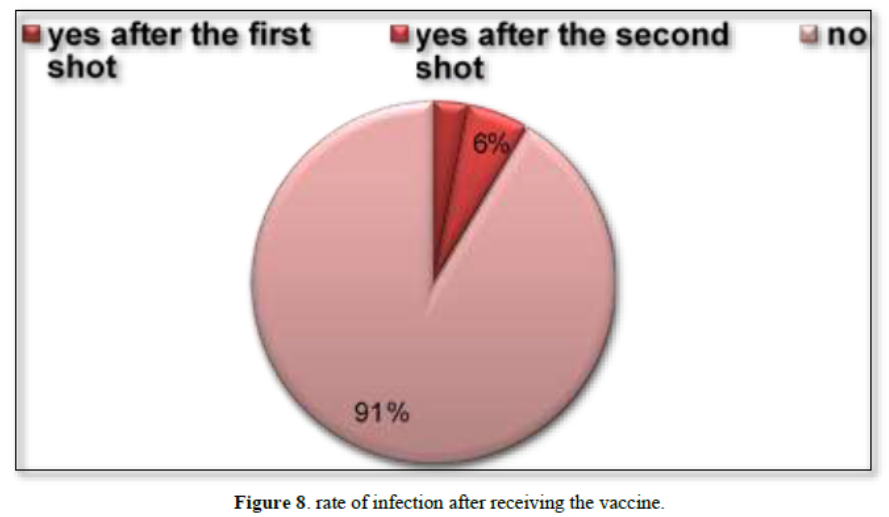
 Participants were answered a question if they got infected after they had the vaccine. Only 4.9% of the respondents got infected after the second shot and 2.81% after the first shot. However, 82.86 did not get infected at all, as shown in Figure 8.
Participants were answered a question if they got infected after they had the vaccine. Only 4.9% of the respondents got infected after the second shot and 2.81% after the first shot. However, 82.86 did not get infected at all, as shown in Figure 8.
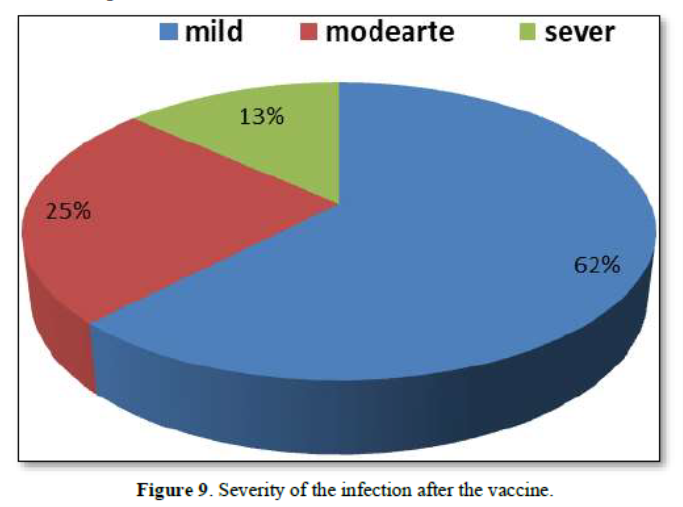
When we asked people about the severity of their symptoms when they were infected with the COVID 19 after receiving the vaccine. A large percentage of the responses had experienced mild symptoms, about 62.2% (84) (Figure 9). While about 13.3% (18) of the respondents had severe symptoms, and 24.4% (33) moderate symptoms (Figure 9). Perhaps infection with the virus and the emergence of somewhat severe symptoms after receiving the vaccine created uncertainty among people about the effectiveness of vaccines.
Do you think the vaccine is safe and effective?
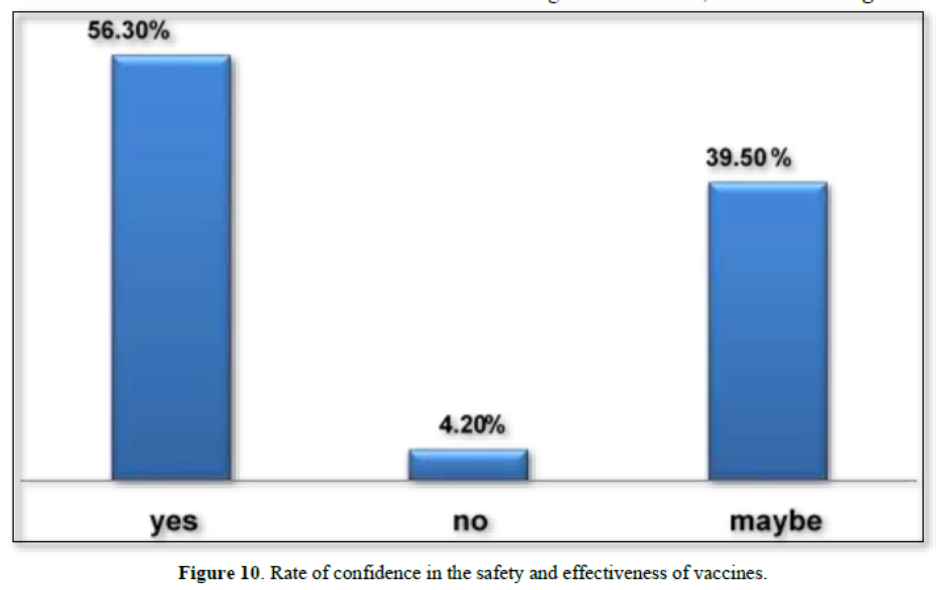
We noticed that 56.3% (440) of participants believe that the vaccine is safe and effective and reduce the possibility of COVID 19 infection. While 39.5% (309) have doubts about the safety and effectiveness of the vaccine and only 4.20% (33) of participants don’t believe that it is safe and effective tool against infection, as shown in Figure 10.
Do you think that who should receive the vaccine are those with poor health only?
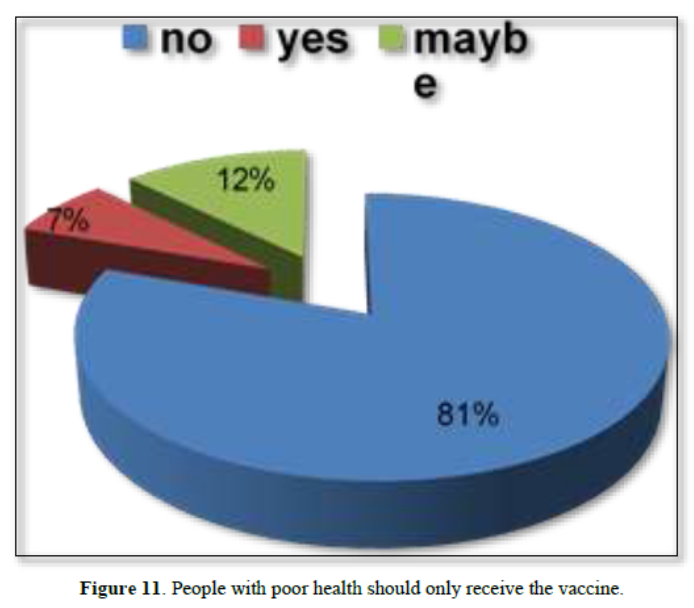
We also found that a very large percentage, 80.1% of people (626), believe that all population, whether old or young and regardless of health condition, should take the vaccine to minimize infection possibility and/or symptoms (Figure 11). While about 7% (59) believes that only those with poor health for example elderly should receive the vaccine and 12.4% (97) of them were not certain about the health conditions of people welling to receive vaccines, as shown in Figure 11.
Do you think that who got infected previously does not need the vaccine?
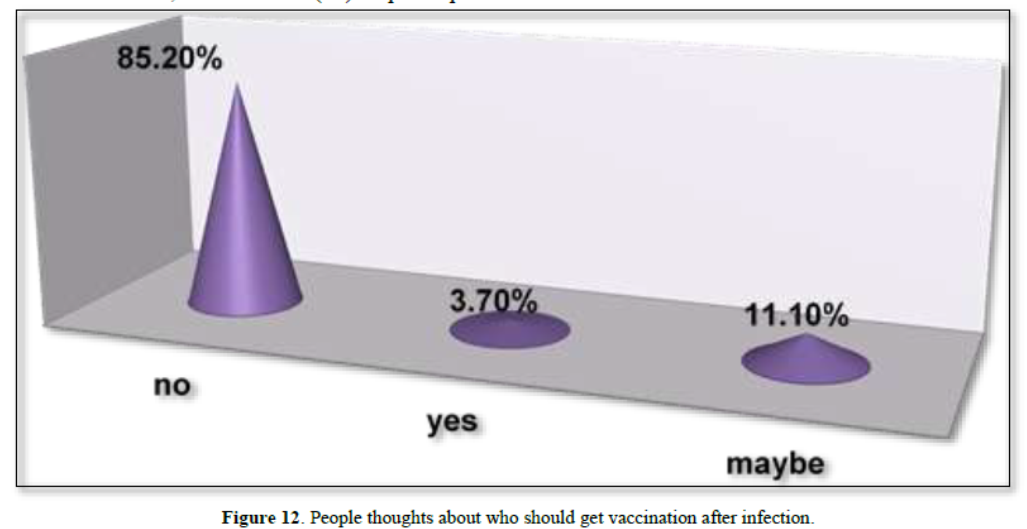
A high percentage of participants, about 85.2%, (666), do not support the idea that those who were previously infected with the COVID 19 do not need to take the vaccine. This means that they are encouraged to receive the vaccine to reduce infection. However, about 11.1% (87) of participants were not sure (maybe) if there is a need to receive the vaccines after infection. This perhaps means that they are still confused about the vaccine. While only 3.7% (29) answered were totally agree that they should not get vaccine after infection. They believe that those who were previously infected have acquired immunity against the disease and there is no need for the vaccine, as shown in Figure 12.
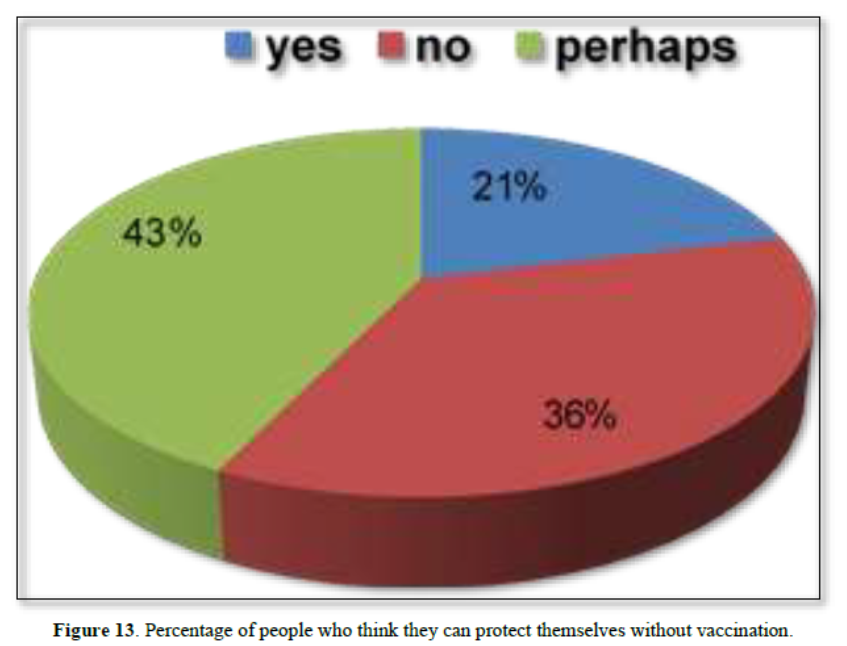
 Can you protect yourself from infection without taking the vaccine?
Can you protect yourself from infection without taking the vaccine?
We also evaluate people believes about protecting themselves from the infection without taking the vaccine. We noticed that about 42.8% (335) of participants were not sure whether they can protect themselves without vaccination (Figure 13). While 36.1% (282) of participants were disagree with this idea, and 21.1% (165) were agree with protection without vaccination, as shown in Figure 13.
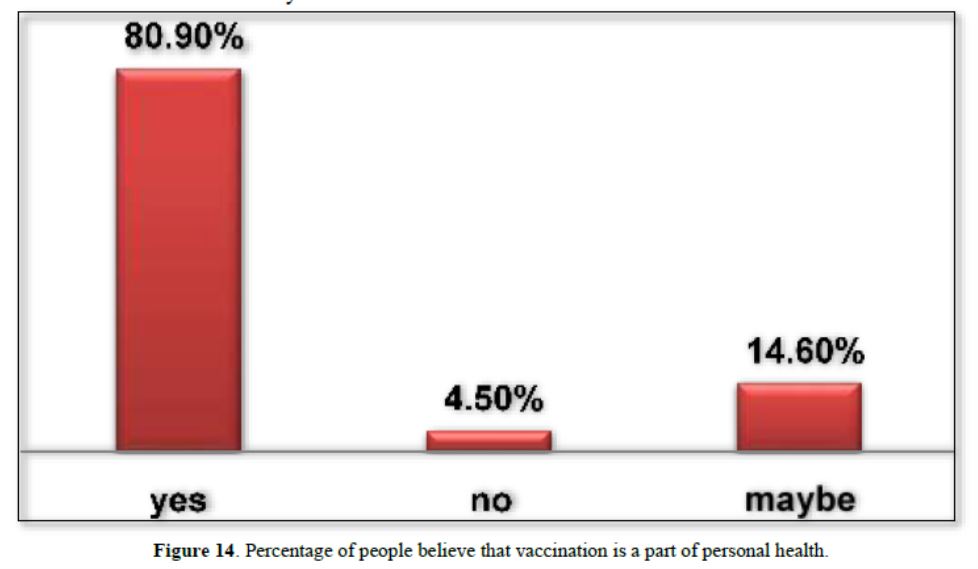
Do you think that getting the vaccine is part of taking care of yourself, and do you advise your family members and friends to take the vaccine?
We also evaluate that whether vaccination is a part of taking care of your personal health and whether your advice others to get vaccines. We noticed that 80.9% (633) agree with this idea (Figure 14). On the other hand, 14.6 % (114) of participants were not fully sure about this practice, and only 4.5% (35) were disagree, as shown in Figure 14.
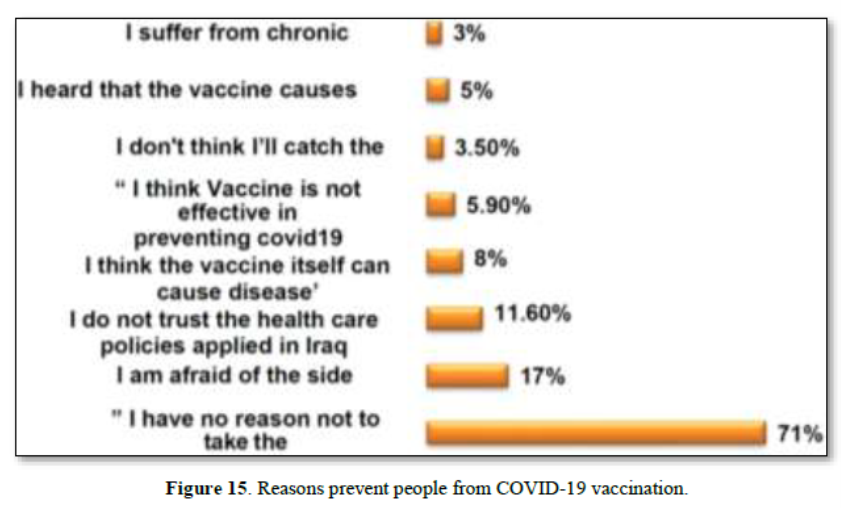
Reasons for not receiving COVID-19 vaccines were also evaluated in the survey. We found that 551 (46.69%) of the respondents answered with “I have no reason not to take the vaccine”; 139 (11.78%) answered with “I am afraid of the side effects” ; 91 (7.71%) answered with “I do not trust the health care policies applied in Iraq”; 59(5%) answered with “I am not sure I think the vaccine itself can cause disease”; 46(3.90%) answered with “I think Vaccine is not effective in preventing COVID-19” ; 27(2.29) answered with “I don't think I’ll catch the virus”; 36(3.05%) answered with heard that the vaccine causes infertility‖; and 24 (2.03%) answered I suffer from chronic diseases, as shown in Figure 15.
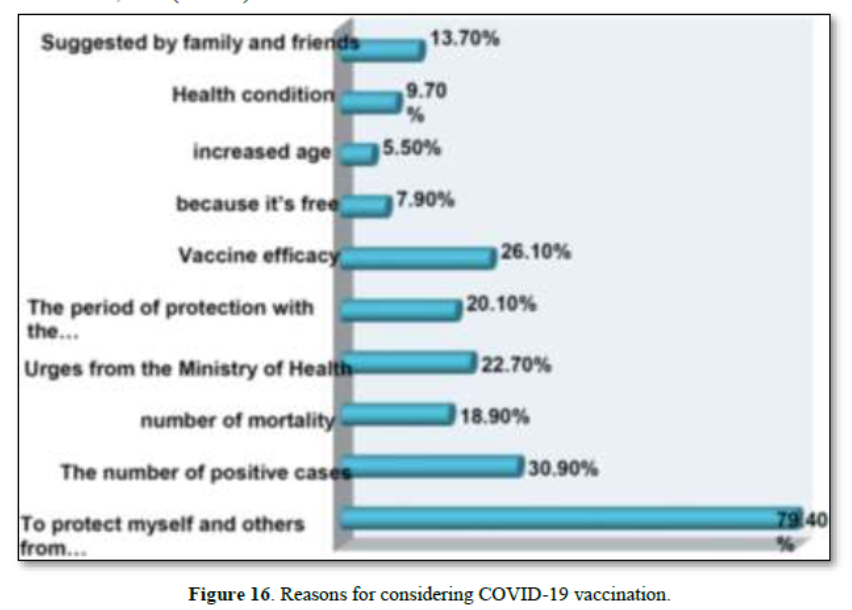
On the other hand, reasons for considering vaccination were also evaluated in our survey. We noticed that most of participants 566 (79.4%) answered with “To protect myself and others from infection” ; 220(30.9%) answered with “The number of positive cases” ;135 (18.9%) answered with “number of mortality”; 162(22.7%) answered with “Urges from the Ministry of Health” ;143 (20.1%) answered with “The period of protection with the vaccine”; 180(26.1%) answered with “Vaccine efficacy”; 56(7.9%) answered with “Because it‘s free”; 39(5.5%) answered with “Increased age”; 69(9.7%) answered with “Health condition” ; and 98(13.7%) answered with “Suggested by family and friends”, as shown in Figure 16.
DISCUSSION
Although wearing masks and social distancing are helpful in minimizing chances of virus exposure or distributing it to the others, these measures are not effectively enough [10]. To protect people from COVID-19 infection, vaccination in the simplest, safest, and most effective method according to the WHO. In addition, COVID-19 vaccines are highly effective in reducing the risk of severe illness and death [5]. Vaccines through enhancing the function of immune system activate our bodies to develop self-protection against the virus [13].
Since 2020, multiple COVID-19 vaccines have been approved for emergency use. These vaccines are safe and effective and, therefore, led governments to actively recruiting people to be involved in the vaccination process. However, global hesitancy towards the vaccines was noticed since the time of vaccines appearance.
In our survey, we found a large variability between people who received both shots of COVID-19 vaccines and those who never took any shots. The percentage of participants who received the two shot was high (73.1%), and rather a small percentage of those who never received vaccination (10.9%). When people were asked about their opinion regarding the vaccine, especially the vaccinated once, they responded that vaccines are safe and effective, and it is the most trusted way to protect against infection. On the other hand, we noticed that others have doubts about the safety and effectiveness of the vaccine (Figure 9).
It is believed that hesitancy against vaccines is based on lack of knowledge, no uncertain about vaccine benefits, and overconfidence on other protective tools, such as masks and hand washing. Moreover, other people feel anxious about vaccination process. This is either due to tangible fears (e.g., of needles or medical settings), worries about adverse effects, or unconscious feelings that vaccines are related with illness or harm. This conception, in a major part, a consequence of misleading information that is actively distributed actively distributed by anti-vaccine groups. Misinformation and conspiracy theories distributed online through social media are major players against vaccination hesitancy [14].
Results observed in our survey regarding the percentage of acceptance and hesitancy were as follows: 81% received the vaccine, 81% believes that vaccination is part of taking care of themselves, 56% believes that the vaccine is safe and effective, a relatively high percentage 70.5% do not have any reservation about taking the vaccine, as shown in Figure 9. A previous study that was conducted also in the Arabian region between 14 January 2021 to 29 January 2021 shows a higher vaccine hesitancy and refusal among Arabian individuals. It has been shown in this study that the lack of vaccines trust and concerns about their adverse effects are the main reasons for higher hesitancy rate [15]. We clearly notice that the percentage of vaccine hesitancy in our study is lower than that of the previous study (Figure 9). This could be related that people different parts of the Arabian world have different perceptions about the vaccination process. It is also possible that the survey duration is longer in our study which could influence on people opinions and become less resistant to accept vaccination. Finally, it is also possible that the individuals in our study from a different economic, education, social levels which could influence on the different findings of the two studies.
It has been noticed that attitudes towards vaccines safety and effectiveness have been markedly changed before and after the broad spectrum of vaccination campaigns. Early attitudes about serious sides effects that could be caused by vaccines, such as death due to blood clots and infertility, were noted in correct and they are merely social media rumors [16]. The lack of trust in pharmaceutical, which is another reason that leads to poor adherence to the vaccination process, was also diminished with the time. Many people believed that the duration was too short for the production of these vaccines and not enough studies were conducted regarding vaccine safety and effectiveness [4].
After the great encouragement from the Ministry of Health, health workers and aware influencers in the media, awareness of the vaccine’s role has been gradually raised. The mandatory of vaccination in some state departments and universities and for foreign travel was also helpful in this regard. Other factors that reduced hesitancy against vaccines include people noticed the lightness of the side effects of the vaccine. These effects could be ranged from pain in the site of injection and fatigue to a slight increase in body temperature. Of course, these symptoms differ from one individual to another, and usually disappear after two to three days.
It is important to mention here that regardless of vaccine type and effectiveness, viruses spread out cannot be merely avoided through vaccination. Vaccine work through enhancing the immune function of our bodies, not more and not to prevent infection. This believe has created misunderstanding among people who do not realize how vaccines work. Clearly, this does not mean that it is impossible that a person might get infected after vaccination. However, the probability of hospitalization and/or death caused by virus infection will be much less in comparison to people without receiving the vaccine [17,18].
In conclusion, our findings support the need to improve knowledge about COVID-19 infection and vaccination through education and awareness programs. Specifically, residents of rural areas should be targeted to optimize COVID-19 vaccine acceptance among the Iraqis population.
ACKNOWLEDGMENT
We are grateful for Zeinab abdulmutalib jabir, Zahraa fahad abdulmajeed, and Sura Hussein Ali for their assistance with studies.
No Files Found
Share Your Publication :